Mental health treatments have come a long way, with options ranging from traditional antidepressants to groundbreaking therapies. Ketamine vs SSRI is a hot topic in mental health circles, as more people seek alternatives to manage depression and anxiety. While both treatments are effective for many, they work in different ways and have unique benefits and risks. Let’s break down these differences to help you make an informed decision.
What is Ketamine and How Does It Work for Mental Health?
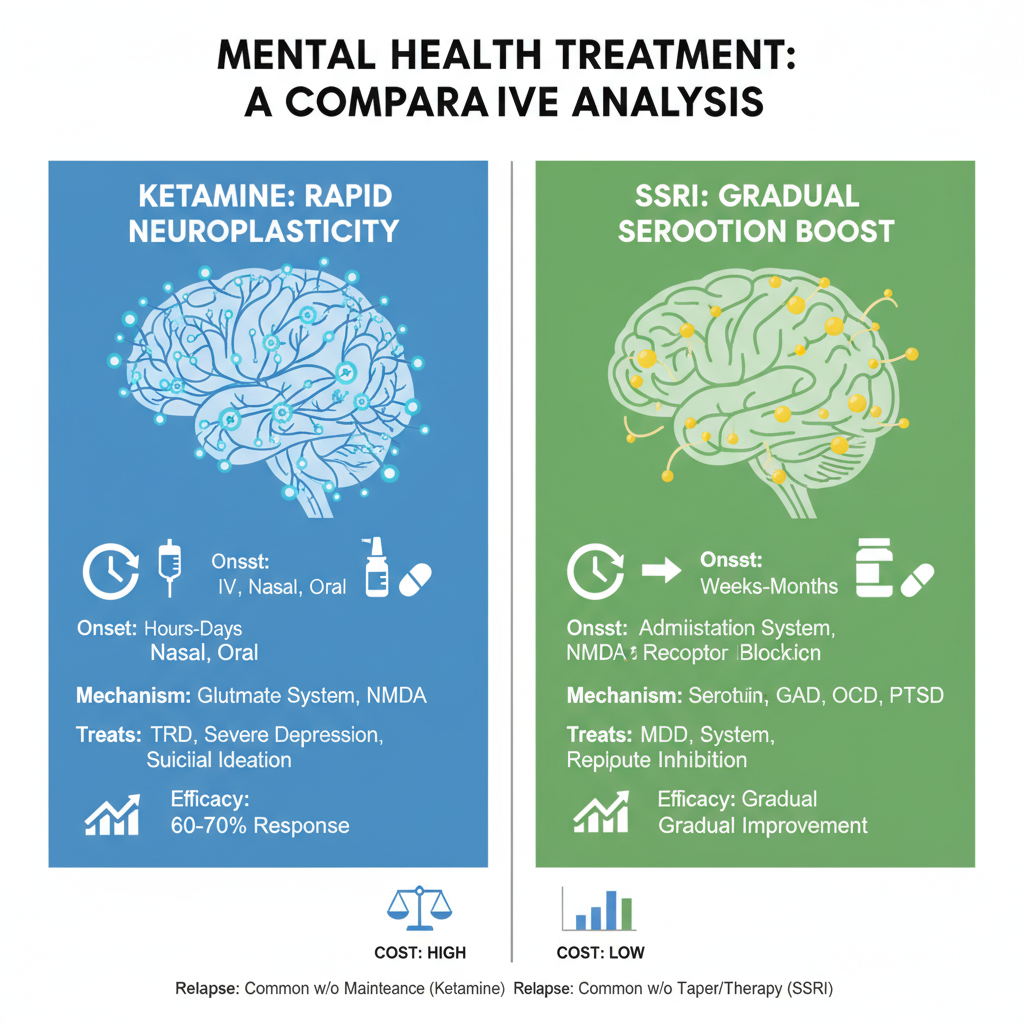
Ketamine, traditionally used as an anesthetic, has recently gained attention for its ability to treat treatment-resistant depression and other mental health conditions. Unlike conventional antidepressants, ketamine works by targeting the NMDA receptors in the brain. These receptors play a key role in regulating mood and neural plasticity.
When administered in a clinical setting, ketamine has been shown to provide rapid symptom relief—often within hours offering hope for those who have not found success with other medications. For many individuals struggling with severe depression, ketamine can be a game-changer, especially when other treatments have failed.
SSRIs: The Long-Standing Solution for Depression and Anxiety
Selective serotonin reuptake inhibitors (SSRIs) have been the go-to treatment for depression and anxiety for decades. Medications such as fluoxetine (Prozac), sertraline (Zoloft), and escitalopram (Lexapro) are all part of this class. SSRIs work by increasing the amount of serotonin, a neurotransmitter, in the brain. This helps improve mood, manage stress, and regulate sleep.
Unlike ketamine, SSRIs require more time to take effect, typically 4 to 6 weeks. They are prescribed for both long-term management and maintenance of depression and anxiety disorders. They are often the first line of defense for individuals diagnosed with these conditions.
Key Differences in Mechanism of Action: Ketamine vs SSRI
Understanding how these treatments work in the brain is essential when considering their benefits. Ketamine vs SSRI differs in how they address neurochemistry.
- Ketamine: Targets glutamate, a neurotransmitter involved in brain signaling. By stimulating the NMDA receptors, ketamine enhances synaptic plasticity essentially rebooting neural connections that affect mood regulation. This results in a rapid antidepressant effect, often within hours.
- SSRIs: Work by increasing serotonin levels in the brain, a neurotransmitter believed to regulate mood, anxiety, and stress. By inhibiting the reuptake of serotonin, SSRIs allow more of it to remain in the synaptic space, improving communication between neurons and improving emotional regulation.
While both treatments impact neurotransmitters, ketamine offers immediate relief compared to SSRIs, which work more gradually over time.
Side Effects and Risks: What to Expect from Ketamine and SSRIs
While both treatments have their advantages, they come with potential risks and side effects.
Ketamine Side Effects
- Short-Term: Dizziness, increased blood pressure, dissociation (feeling detached from reality), nausea, and confusion. These side effects generally resolve quickly after the treatment session.
- Long-Term: Prolonged use of ketamine may cause bladder issues or cognitive impairments. However, these risks are typically associated with recreational abuse rather than therapeutic use under medical supervision.
SSRIs Side Effects
- Short-Term: Nausea, insomnia, sexual dysfunction, weight gain, and headache. These side effects often improve after the first few weeks of treatment.
- Long-Term: Some individuals experience persistent sexual side effects or emotional blunting. However, SSRIs are generally considered safer for long-term use compared to ketamine.
Effectiveness: Ketamine vs SSRI in Treating Depression
Ketamine’s Quick Action
One of the key advantages of ketamine is its rapid onset of action. Unlike SSRIs, which require weeks to show effects, ketamine can relieve depressive symptoms within hours or days. This makes it particularly beneficial for people with severe depression or those at risk of suicide. Studies have shown that around 70% of people with treatment-resistant depression experience significant improvement after a single ketamine treatment.
SSRIs’ Long-Term Benefits
SSRIs, on the other hand, are more suited for long-term management of depression and anxiety. While they take time to show results, they can help individuals maintain a steady mood and reduce the likelihood of relapse. Research indicates that SSRIs are effective for many individuals and can significantly reduce the frequency and severity of depressive episodes over time.
Choosing the Right Treatment: Ketamine vs SSRI for Your Needs
When deciding between ketamine vs SSRI, the best choice depends on your situation:
- Ketamine: Ideal for individuals who need immediate relief from severe depression or those who have not responded to traditional treatments. Ketamine may also be beneficial for people with suicidal thoughts or severe depressive episodes who require rapid intervention.
- SSRIs: Better suited for individuals seeking long-term management of depression or anxiety. They are generally the first-line treatment and are effective for people with generalized anxiety disorder, chronic depression, and social anxiety.
Conclusion:
Both ketamine vs SSRI have proven their value in mental health treatment, but the choice ultimately depends on your specific needs. Ketamine offers rapid relief and may be a lifeline for individuals with severe depression, while SSRIs provide a long-term solution for managing mood disorders and are typically the first treatment choice.
If you’re struggling with mental health issues, it’s important to consult with a healthcare provider who can guide you through the decision-making process. They can help you determine the best treatment based on your symptoms, medical history, and overall goals. Whether you choose ketamine, SSRIs, or a combination of treatments, the key is to find a solution that works for you.